In the sterile hum of a Boston research lab, Dr. Kevin Hill stared at a mountain of data—over a thousand studies piled like unanswered prayers. As director of addiction psychiatry at Beth Israel Deaconess Medical Center and a Harvard professor, he’d seen the green wave crash over medicine: patients pleading for cannabis to ease their chronic pain, cancer nausea, or epileptic seizures. “It’s a miracle plant,” they’d say, echoing dispensary whispers. But Hill’s screens glowed with a harsher truth. “We reviewed the totality of the evidence,” he told Newsweek in a bombshell review that lit up headlines, “and beyond the FDA-approved indications, the evidence for cannabis and cannabinoids as a medical treatment is limited.”

It started innocently enough, back in the early 2010s, when states began legalizing medical marijuana like Colorado in 2000, promising relief for the suffering. By 2025, 27% of adults in the U.S. and Canada were using it medicinally, with 10.5% turning to CBD oils for everything from anxiety to insomnia. Sarah Jenkins, a 42-year-old teacher from Seattle, was one of them. Diagnosed with fibromyalgia in 2018, her world shrank to a cocktail of opioids and endless doctor visits. “The pain was a constant scream in my muscles,” she recalls, her voice steady now but laced with the echo of those dark days. Desperate, she got her medical card and started with edibles—low-dose gummies promising sweet escape. At first, it worked: mornings dawned without the vise grip, afternoons stretched into walks with her kids. “I felt human again,” Sarah says. Friends cheered; social media buzzed with #WeedHeals testimonials. But whispers of doubt lingered—why did her anxiety spike on weekends? Why the foggy mornings after?
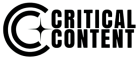
Sarah’s story mirrored millions, but science lagged behind the hype. Hill’s team dove deep, prioritizing gold-standard randomized trials and meta-analyses. What they found chilled the room: solid proof for just a handful of uses, like FDA-approved CBD for rare epilepsies or dronabinol for chemo-induced nausea. Chronic pain? “The evidence is not strong,” Hill admitted. For epilepsy beyond specifics, appetite loss, or sleep woes—crickets. Worse, the risks piled up like storm clouds. Nearly a third of medical users spiraled into cannabis use disorder, that gnawing dependency turning relief into chains. Daily inhalers faced heart alarms: higher odds of attacks, strokes, even coronary disease. Cancer patients puffing away? Their immunotherapy might falter, eggs and embryos at risk for would-be moms.

“I was gaslit by the glow-up,” Sarah laughs bitterly, scrolling old posts from her vape-filled haze. In 2022, after two years of “treatment,” her heart raced during a routine checkup—docs linked it to her nightly joints. Fertility dreams with her partner? Derailed by studies showing THC’s sneaky sabotage. “They sold us salvation in a smoke cloud, but no one mentioned the carcinogens or the addiction hook,” she says. Dispensaries, unregulated wild west outposts, peddled inconsistent doses—high-THC bombs without labels or limits. “We customarily expect medicinal drugs to guarantee consistency,” Carnegie Mellon’s Jonathan Caulkins warned. “With cannabis? It’s roulette.”
The reckoning hit in late 2025, as Hill’s review dropped amid Senate battles to ban rogue THC edibles. Experts rallied, but not in unison. Mount Sinai’s Yasmin Hurd nodded gravely: “It confirms what we’ve known—insufficient evidence for most conditions.” She urged caution: “Start low, go slow, and only after conventional therapies fail.” UC San Diego’s Igor Grant pushed back gently: “The review’s useful, but it leans heavy on negatives. Risks are real, but protocols can manage them.” Still, the chorus swelled: Cannabis wasn’t the panacea; it was a third-line gamble, laced with unknowns.

Sarah quit cold in spring 2023, swapping buds for yoga and therapy. The withdrawal was hell—insomnia clawed nights, irritability snapped days—but clarity emerged like dawn after fog. “My pain’s managed with PT and meds now, no heart flutters, no dependency dread,” she shares in a TikTok that’s racked up 500K views. “I got my life back by facing the facts.” Today, she advocates in patient forums, urging: “Demand evidence, not echoes. Talk to docs, not dealers.”
Hill’s wake-up call rippled wider, forcing a national pause. As legalization surges—38 states green by 2025—his work spotlights the gap: hype versus hard data, hope versus heart risks. “The adverse effects are becoming well-defined,” Hill says, “and most often, risks outweigh benefits.” Yet in that balance lies progress: calls for rigorous trials, FDA oversight, and doctor-patient dialogues over dispensary deals.
In a world chasing quick fixes, Sarah and Kevin remind us: True healing demands unflinching truth. One puff at a time, we’re learning—not all green is gold. What’s your take on medical cannabis? Drop it below—we’re unpacking the haze together.